Medical Disclaimer
This article is provided for informational purposes only and should not be considered medical advice. Always seek the guidance of qualified healthcare professionals regarding any questions you may have about a medical condition or treatment.
Anoxia at birth refers to a critical situation in which a newborn experiences a complete absence of oxygen during or immediately after labor and delivery. This condition can arise from various complications—ranging from umbilical cord issues to placental problems—and carries significant health implications for the infant. In this article, we will discuss the principal causes of anoxia at birth, highlight the key risks and lasting effects, and explore various medical interventions that can improve outcomes for affected newborns.
If you’re unfamiliar with the broader concept of anoxia and how it affects the body, consider reading our foundational article:
Anoxia Explained: Causes, Effects on the Body, and Key Treatment Approaches.
1. Understanding Anoxia at Birth
1.1 What Exactly Is Anoxia at Birth?
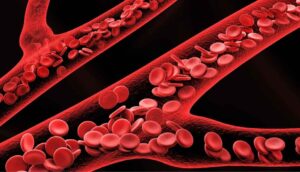
Anoxia at birth occurs when a fetus or newborn is deprived of oxygen, even for a brief period. While mild oxygen deprivation (hypoxia) can also be harmful, anoxia represents the complete lack of oxygen supply. If not quickly resolved, it can lead to widespread organ damage, particularly in the brain.
Common Causes:
- Umbilical Cord Compression: A prolapsed or twisted cord can abruptly stop the flow of oxygen-rich blood.
- Placental Abruption: The premature separation of the placenta from the uterine wall can severely limit oxygen exchange.
- Maternal Health Issues: Low blood pressure, respiratory failures, or maternal infections may compromise oxygen delivery to the fetus.
- Prolonged Labor or Delivery Complications: Difficult deliveries, including those requiring emergency procedures, may increase the risk of anoxia at birth.
Note: While these are the most frequent causes, any event that inhibits normal circulation or breathing during the delivery process can trigger neonatal anoxia.
2. Key Risks and Immediate Consequences
2.1 Neurological Damage
The brain is highly vulnerable to oxygen deprivation. Within minutes, neurons can begin to die, leading to potential long-term neurologic deficits or, in severe cases, neonatal death. Early symptoms may include:
- Low Apgar scores
- Weak or absent reflexes
- Seizures
2.2 Potential Organ Damage
Although the brain is most at risk, other organs—like the heart, kidneys, and liver—can also suffer from an insufficient oxygen supply. Hypoxic-ischemic encephalopathy (HIE) is a condition often associated with anoxia at birth, where multiple systems may be compromised.
3. Lasting Effects of Neonatal Anoxia
If an infant survives the initial crisis, there may still be long-term complications that emerge over weeks, months, or even years.
3.1 Developmental Delays
Children who experience anoxia at birth often face:
- Speech and Language Delays: Difficulty in forming words or understanding language.
- Cognitive Challenges: Problems with memory, attention span, and learning new tasks.
- Behavioral Issues: Hyperactivity or social interaction difficulties.
3.2 Motor and Cognitive Impairments
In more severe cases, anoxia at birth can lead to cerebral palsy or other permanent motor disorders. Early intervention programs and consistent therapy can, however, help mitigate these effects.
Related Reading:
Discover more about the broader topic of brain damage from oxygen deprivation in our article on
Anoxic Brain Damage: Understanding Oxygen-Deprivation Injuries and Recovery Options.
4. Medical Interventions and Treatments
4.1 Immediate Steps Post-Delivery
- Resuscitation: In cases where the newborn is not breathing or has a weak heartbeat, immediate neonatal resuscitation is crucial.
- Ensuring Oxygen Supply: Supplemental oxygen via respiratory support systems can rapidly stabilize oxygen levels in the infant’s bloodstream.
4.2 NICU Care and Monitoring
Many newborns who experience anoxia at birth require specialized care in a Neonatal Intensive Care Unit (NICU). There, medical professionals can:
- Monitor Vital Signs: Track oxygen saturation, heart rate, and brain activity.
- Regulate Temperature: Maintain a stable body temperature to reduce metabolic stress.
- Manage Fluids and Electrolytes: Ensure balanced hydration and avoid fluid overload that could worsen edema or organ stress.
4.3 Therapeutic Hypothermia
Also known as cooling therapy, this approach lowers the baby’s body temperature for a set period (usually 72 hours) to slow metabolic processes and minimize cellular damage in the brain.
4.4 Follow-Up and Long-Term Therapies
Early and consistent therapeutic interventions can make a significant difference in a child’s prognosis:
- Physical and Occupational Therapy: Aids in developing muscle tone, coordination, and daily living skills.
- Speech and Language Therapy: Helps address communication hurdles if cognitive or speech centers were impacted.
- Behavioral and Cognitive Assessments: Identifies challenges early on, allowing for targeted educational strategies.
Learn More:
For insights on how anoxia impacts overall prognosis and factors that can influence survival or recovery, read
Anoxic Brain Injury Prognosis and Survival Rates: Key Factors that Shape Recovery.
5. The Long-Term Outlook
5.1 Factors Influencing Prognosis
- Severity of Oxygen Deprivation: Longer periods of anoxia often correlate with more extensive damage.
- Time to Intervention: Rapid resuscitation and immediate medical support can drastically improve outcomes.
- Underlying Maternal Health: Pre-existing conditions like hypertension or diabetes in the mother can complicate newborn recovery.
- Post-Discharge Support: Access to quality medical follow-up, therapy programs, and family education plays a huge role in a child’s developmental trajectory.
5.2 Quality of Life
Although anoxia at birth can pose significant challenges, many children go on to lead fulfilling lives, particularly with robust early intervention, ongoing medical care, and strong familial support. Parents and caregivers are encouraged to work closely with pediatric specialists, neurologists, and therapists to optimize each child’s potential.
Conclusion
Anoxia at birth presents a formidable challenge, with the potential to affect multiple organs—most critically, the brain—within minutes. Yet, advances in neonatal care and medical interventions such as therapeutic hypothermia have improved the outlook for many newborns. Early detection, prompt treatment, and committed long-term follow-up can significantly mitigate the lasting effects of oxygen deprivation.
If you’re looking to better understand the broader concept of anoxia and how it applies to both newborns and adults, check out our in-depth overview:
Anoxia Explained: Causes, Effects on the Body, and Key Treatment Approaches.
For more detailed insights into the recovery process following oxygen deprivation, you may also find our article on Anoxic Brain Damage: Understanding Oxygen-Deprivation Injuries and Recovery Options helpful.
Remember: Always consult with qualified healthcare professionals for personalized advice if you suspect or observe any signs of anoxia at birth. Immediate medical intervention can make a life-changing difference.